Transplant Evaluation.
Did I just say that?
Or did my head shake and wake me from a dream.
Maybe some sort of denial is preventing me from actually believing that my doc is suggesting it’s “T” time. Time to think about being listed for a double lung transplant.
Now I have always known that the transplant decision was in my future. But it always seemed so far off in the distance. A place I saw myself physically and slowly moving towards, knowing that the time would be crystal clear in my thinking. So why do I feel like the timing is not right? I don’t feel THAT sick yet. Usually, lung transplantation is recommended when a patient’s lung disease is so severe that their chance of surviving with their original lungs is estimated to be two years or less. Am I actually there? The lung transplant itself carries it’s own risks and set of survival rates. About 1/2 of recipients will last 5 years or more post transplant. So of course, it would only make sense that I would want to get the most use of my own God given lungs, for as long as they are still able to function. After all, they have given me 54 years, and counting, of life.
Yes, I have been pretty sick this year, with 4 hospitalizations in 8 months, which is too much. My left lung is at end stage lung disease, there’s just not much left to function. My right lung is still functional, still feels clear. But I, of all people, should know not to get to comfortable in that thinking. To think my right lung will carry me, for a while longer. De ja vu.
I was at that place 11 years ago, when MAC was driving, 100 MPH and taking me to the grave. I was dying and I knew it, I could feel it. I had all the symptoms of end stage lung disease . . . constant, unrelenting infection and coughing, fevers, chest pain, high heart rate, losing weight, couldn’t eat, no energy, couldn’t do anything! My left lung was consumed with MAC in places while my right lung was fine. Wedge resection surgery was my last ditch effort to remove all the life sapping sections of my left lung . . . hell bent on killing me. Lung transplant surgery was still a fairly new procedure at the time, so wedge resection was decided instead. My surgery worked, it restored my health and life, it was my saviour. It gave me 10+ years of quality life until now, some of the best years of my life. I never once regretted having that surgery, I’d do it again in a heartbeat. It was high risk at the time, but a risk I was willing to take. Either that or die.
The decision for my last surgery are the same reasons as for transplant now. My left lung will eventually spread the frequent infections to my right lung. My right lung is keeping me going at this point. It too is progressing downhill, just not as fast as my left. As Dr. R tells me, transplant (Tx) will be my safety net when my right lung begins to fail. It is a given guarantee that it will happen, just don’t know when. For now, Dr. R wants to play it safe, get all the Tx testing out of the way, while I’m still healthy enough and put me active on the list me when the timing is right. *shakes my head again*
The Tx coordinator and the Tx social worker both visited my room for introductions and some lengthy talks. They basically described the process, how it works, answered any questions I had, evaluated my mental stability and home life, wanted a complete ‘life’ history both medically and just in general how I’ve lived my life. This is so important because a Tx is such a life changing experience they want to make darn sure that I can mentally adjust to the changes and responsibilities of upkeep post Tx. I have many more meetings to be scheduled with other members of the Tx team, including the surgeons. All this will happen when my evaluation testing is complete. Then a determination will be made if the timing is right for me to be actively listed or wait a while longer. I just have to put trust in the docs that they know the right time based on my test results. Ugh, it is all overwhelming for me.
While I was in house, I got most of the physical testing I needed done.
Here are the tests I completed:
1. Complete PFT aka Spirometry. Pulmonary function testing measures lung volume, small airways, % of lung function, and liters of O2 I can take in and out in one big breath. A complete explanation is here
2. The 6 minute walk test. Simply, see how far and fast I can walk in six minutes, up and back in the hospital hallway. They also measured my O2 sats to see if I need supplemental oxygen. The lowest my sats went were 91, I passed. :) Anything under about 90, indicates supplemental oxygen may be necessary.
3. The blood sucker test. I call it this because the Phlebotomist from lab came into my room and stole about 22 vials of blood. A multitude of tests are determined by my blood. Blood typing for donor matching, kidney function, liver function, vitamin levels, drug and tobacco screens, and to rule out other maladies such as active chickenpox, TB, Epstein-Barr virus, hepatitis, herpes, AIDS, & HIV.
4. Arterial blood gas aka ABG. A blood test taken from an artery instead of a vein - ouch! ABG is mainly used in pulmonology, to determine oxygen and CO2 exchange levels in the blood related to lung function.
5. 24 hour urine collection. Tests kidney output and function.
6. Chest Xray
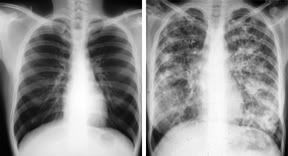
These are not my xrays.
The left xray is of normal lungs, the right are CF lungs, they turn white when damaged.
7. Chest CT scan
8. Electrocardiography aka EKG. Used to measure and diagnose abnormal rhythms of the heart.
9. Echocardiogram with bubbles. Ultrasound of the heart while injecting saline microbubbles into the venous system. This shows any abnomalities in the cardiovascular sytem such as diseases of the heart valves, any damage to heart tissue, and severity of any present coronary artery disease.
10. Right heart catheterization - to check for artery lung pressure. I described this procedure in my prior post.
Tests I still have to do:
1. Left heart catheterization with angiogram, scheduled for 6-14. Assesses any cardio damage or coronary blockages. I only need to have this done because I’m over 50. If the test shows any abnormalities in my heart, such as a small leak or hole, it will be fixed during transplant surgery. Barring any complications, this will be outpatient, but will require me to spend a full day at USC.
2. Complete and current gynecological exam - I was due for this anyway and have an appointment scheduled in July.
3. Mammogram - ditto for this, appointment scheduled in July.
4. Complete oral exam - I’ve been waiting for authorization for this appt to be checked at the USC Dentistry school.
Between all the physical tests and mental ping pong I played, this hospitization was exhausting. I’ve been out now 2 weeks, and I finally feel somewhat normal again. I’ve been reading transplant info whenever I can and making lists of ?? I have for the Tx team. I’m also going to attend a Tx support group at USC the first Tuesday of every month. I know several online groups too, which I plan to start participating in. And lastlly, I have other CF friends who have had a Tx or are on the waiting list. I will defintiely pick their brains too.
One more step of my journey, that I must embrace. I can only think positive thoughts that the Tx will work out great for me. I’m hoping for many more years of good life left, to spend with my family and friends.
Now if only I can finish wrapping my head around the whole idea and accept it wholeheartedly. But I know, I will, it takes time. :)















2 comments:
That left normal xray almost looks fake doesn't it?
I can't believe all that happened during your last hospital stay. Way too much Jodi!
Big hugs to you ~
LOL, Kelly! I know huh? We're so used to seeing the white ones, unfortunately. :( We can only wish ours looked so black! :)
Post a Comment